
A Total Knee Replacement (TKR) procedure, also referred to as Total Knee Arthroplasty (TKA), is a surgical procedure which involves resurfacing your knee joint and replacing the arthritic parts with artificial metal or plastic prosthesis components.
These components move together to allow near to normal function in the knee.
Who is suitable for a Total Knee Replacement?
People with a stiff, painful knee that makes it difficult to perform even the simplest of movements and interferes with daily activities despite trying other non operative measures such as anti inflammatory medication, activity modification and joint rehabilitation exercises without significant improvement may be candidates for Total Knee Replacement Surgery.
Your knee surgery is recommended only after careful diagnosis of a knee problem, including your degree of pain and lack of mobility.
Further testing may be required if the diagnosis is not clear such as:
- X-Ray – this needs to be weight bearing. The use of a weight-bearing x-ray can determine the extent of the degeneration in the joint.
- Blood Test – this may determine if there is inflammatory arthritis or infection in the hip.
- Scanning and MRI – this can determine if you have avascular necrosis.
- Bone Mineral Density – this determines the condition of the bone or the presence of osteoporosis.
Your hip surgery is recommended only after careful diagnosis of a hip problem, including your degree of pain and lack of mobility.
Benefits of a Successful Total Knee Replacement include Reduction in Knee Pain, Recovery of Mobility and Improvement in Quality of Life
What implants are used?

Up to three bone surfaces may be replaced in a total knee replacement procedure with highly biocompatible implants consisting of plastic and metallic components.
The Femoral Component: This metal implant curves around the end of the femur (thighbone). It is grooved so the kneecap can move up and down smoothly against the bone as the knee bends and straightens.
The Tibial Base Plate: This is typically a flat metal platform with a cushion of strong, durable plastic, called polyethylene. Some designs do not have the metal portion and attach the polyethylene directly to the bone. For additional stability, the metal portion of the component may have a stem that inserts into the center of the tibia bone.
The Patellar component: This is a dome-shaped piece of polyethylene that duplicates the shape of the patella (kneecap), replacing the cartilage function and allowing the thigh and shin bone to slide on each other.
All components are designed so that metal always contacts with plastic. This provides smooth movement and results in minimal wear.
How is a TKR procedure performed?

Knee replacement surgery requires the resurfacing of the bony surfaces of the knee joint. An artificial knee joint is designed to fit over the edges of the joint and to replace the painful joint with one that can be used pain free.
The surfaces of the thigh and and shin bones are replaced with high resistant metallic components called the femoral component and tibial baseplate. Between the femoral component and tibial baseplate a plastic insert is implanted. This replaces the cartilage function allowing the thigh and shin bone to slide on each other. It is not to remove the whole joint, but merely to resurface the diseased or traumatized bony edges.
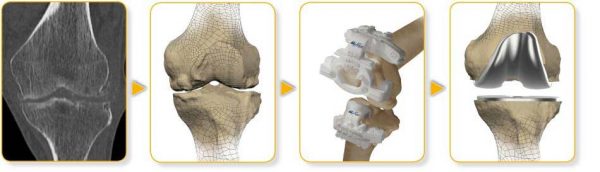
Technical advances have given us new materials and new instrumentation to replace your problem knee. Professor Kohan prefers to perform the knee replacement using patient specific instrumentation for most patients unless there is a specific reason otherwise. This involves analyzing a diagnostic image of your leg and creating a surgical instrument in collaboration with a team of engineers that is tailored specifically to fit the exact shape of your knee.
This Patient Matched Technology enables precise preparation of your bone in surgery for accurate implanting of the prosthesis leading to a less traumatic procedure and to ensure the knee replacement is well aligned.
Once Professor Kohan has diagnosed that a Total Knee Replacement procedure is needed you will be required to have a CT scan of your leg at least 3 weeks prior to your scheduled surgery date.
A plastic 3D model is then created using the image of the CT scan. This enables Professor Kohan to select the best implant for you. Using the 3D model of your knee Professor Kohan then, in collaboration with a team of bio-medical engineers develops the surgical instruments to be used on your knee.
Professor Kohan will receive these patient matched instruments along with a plastic replica of your knee prior to your surgery date.
The procedure is performed as an inpatient meaning you will stay at the hospital overnight. The operation itself will take approximately 3 hours.
Incision: 15-20cms in length and it will run over the top of your knee joint. The incision can take a few weeks to settle down.
There will be a fine catheter in your knee. This is used to inject medications directly into the knee joint to relieve pain. You will also have a drip in your arm. This drip supplies you with fluid and blood if you need it.
What happens after a Total Knee Replacement procedure?
Immediately after surgery, you will wake up in the recovery room. You may feel a bit groggy. Professor Kohan and his staff will monitor you, checking your blood pressure, temperature and pulse. Dr Kerr will also assess your pain level. Post-operative x-rays will be performed in recovery.
After 45 minutes – 1 hour you will then be transferred back to your room on the ward.
When you arrive to your room, you will have:
- A compression garment around the operation site to apply pressure there. This is removed 24 hrs after surgery.
- A pain catheter which will be removed before discharge. We inject local anaesthetic through this to maintain the pain relief.
- TED Stockings (knee high white stockings) on your legs which must be worn for 2 weeks post procedure.
- A drip in your arm. This will provide hydration and blood if you need it
Approximately 2 hours after surgery a physiotherapist will get you out of bed and help you walk for the first time with your new knee.
Your hospital stay will be a combination of rest and rehabilitation.
In the first week following surgery you may experience:
-
-
- Swelling – From your thigh down into your foot is common. This at times may be quite marked. The swelling will increase for the first few days after surgery and will gradually diminish. Some swelling can be present for 12 months or so. The swelling may be diminished by walking as the muscle function will push the fluid away. When you stop walking, the limb should be elevated above the level of the hip.
- Bruising – Marked bruising can be found in some patients. This can be found from your thigh down into your foot. At times the bruising can be quite dramatic but it will resolve. It is the result of some residual bleeding making its way to the surface. The body will eventually remove the bruising. It is also the result of the blood thinning tablets you will be taking.The blood thinning tablets will tend to make the bleeding after surgery a little more marked because the blood clotting is impaired. This is however preferable to developing a blood clot.
- Blistering – On occasions blisters will develop near the operation and possibly above it. The blistering is due to surface fluid. It looks dramatic but it is of no consequence and always resolves. One cause may be the bandage rubbing on the skin. Sometimes, when the blood dries in the bandage it can be like cardboard and rub on the skin producing these blisters. We change the bandage after about a week but would prefer not to interfere with that earlier because of the risk of infection. After about a week the wound is sealed enough to be a reasonable barrier against infection. Another cause for the blistering is tissue swelling. This is associated with the bruising and is a result of fluid leaking into the skin. These blisters always go away. They may burst and leak fluid and again the appearance may be dramatic. Sometimes if they are large we may burst them. This is so that the dressings sit more comfortably.
- Muscle soreness – Your muscles can feel stiff and sore to touch. During the operation some stretching and pulling of the muscles occurs. This may result in some pain like a corked thigh. Occasionally you may feel cramps and spasms. The discomfort however will resolve and activity such as walking, stretching, physiotherapy, etc, will help to speed the improvement.
- Heat – The operated site may feel hot and the heat may last for 12 months. As part of the healing process the operation site requires more blood supply from the body and it is this extra blood supply which is the cause of the local heat.
-
For the first 2 weeks after surgery your activity level is usually limited however you will be able to walk independently, use the bathroom and perform normal activities of daily living. It is important however, to keep on trying to use the knee as normally as possible.
After 6 weeks you will be able to engage in moderate activities, i.e. driving a car and climbing stairs.
Within 8 weeks you will have resumed most of your normal activities. Complete surgical healing takes 6 – 8 weeks but sometimes longer if the arthritis was very severe or the knee very deformed. During this time some swelling and discomfort is normal and should be manageable with the prescribed medication.
Precautions following TKR surgery?
Precautions to take following knee surgery include:
-
-
- Avoid chairs that are low.
- Avoid slippery surfaces.
- Avoid twisting your knee for 6-8 weeks after surgery.
- Avoid siting in the same position for long periods. 45 minutes at a time should be enough. Sitting for long periods increases the likelihood of stiffness.
-
Incision Care
The incision is sutured with skin staples which will be removed 10-12 days after surgery. You will have a firm bandage from your foot to your thigh following surgery which is usually removed on day 5 at your first post op appointment.
The nurses in the hospital will help you change the dressing if needed before you leave the hospital.
You must not get the incision wet until the staples are removed – a sponge bath instead of a shower is therefore recommended for 5 days post surgery.
You may shower after the sutures are removed but may not bathe or swim for 2 more weeks after that.
Your second post-op appointment is to remove the skin clips from your wound. Some swelling and warmth on and around the incision area is expected. If you develop increased redness, drainage or a fever please call the office immediately.
Bruising around the thigh area is also common. It may extend down into your ankle and should resolve in 10 – 14 days.
You may apply Vitamin E or some moisturizing lotion on and around the incision area after the staples have been removed.
Walking
Upon discharge from hospital you will be walking with crutches. You may discontinue using crutches after being assessed by Professor Kohan at your postoperative visit. After this time you may use a cane or if you feel confident you may discontinue using any walking aids at all.
For the first 2 weeks following your procedure you may go up and down stairs as needed but only straight legged. After this time there should be enough flexibility and repair from the muscles around your knee to walk relatively normally.
Expectations
Each individual has his/her own set of expectations. Each patient is treated as an individual with general health, age and attitude considered.
An important thing to remember is that you are not sick. You have a problem with your knee that needs to be fixed.
Getting back on your feet after surgery is the most important goal. ‘Motion is Lotion.’
Will Physiotherapy be required?
Gentle exercises help strengthen the muscles around your new knee and regain your knees range of motion.
As soon as possible your physiotherapist helps you start walking a few steps at a time to promote healing. As you progress from crutches and then to a cane you may feel somewhat off balance at first. Gait training helps you regain confidence and your normal walking motion before going home.
Results of a knee replacement are classified as excellent if activities of daily living can be performed without pain or restrictions. (This does not include running sports). Results are classified as good if occasional mild pain occurs and only slight restrictions of movement are present.
For the past 5 years studies have usually recorded 95% good to excellent results.
Your prosthetic knee can wear out or loosen and may require replacement if necessary. On the other hand, people live longer now and you may out-live your new knee. Regular review is recommended.
In order to reduce stiffness and obtain maximum function of your knee it is important to maintain a good balance of rest and exercise. Listen to your body, too much activity will produce increased swelling, and/or pain, too little will prolong your recovery, and/or limit your knee mobility.
To promote circulation, remember to do your ankle, foot stretching exercises regularly.
On the second day post surgery, remove the knee brace and begin moving the knee and walk, as your knee will allow. The fourth day after surgery you may begin your leg exercises.
Knee Stretching:
Sit in a chair so that your bottom is at the back of the chair; place your feet on a phone book.
Cross your legs at the ankles (good one over the operated leg). Push back leg with front leg until stretch is felt and hold for 15 seconds.
Relax
Raise foot of operated leg, straightening it out and hold it for 15 seconds. Repeat 15 times.
Relax
Do these exercises 3 – 4 times a day. Continue doing these exercises until you return to your normal activities.
Estimate of Fees
Generally our ‘Estimate of Fees’ is accurate however, on occasion unforeseen circumstances can arise during the operation which may require additional medical services or a different, more costly prosthetic device to be used. If this happens there may be additional costs to you that are not covered by the estimate.
This will be fully explained to you after the operation should it occur.
Professor Kohan’s Surgical Fees
Medical Item No: 49518
Surgical Assistant Fees
The surgical assistant fees will either be billed to you directly or Professor Kohan will bill you on his behalf.
Medicare Item No: 51303
Anesthetic Fees
You will meet with Dr Kerr, the anesthetist before your operation so that you can obtain an estimate of his fees. These will be billed to you directly.
Medical Item No’s : 17620, 17690, 21214, 23111, 22045, 18225
There will be 2 ‘no charge’ consultations after your Total Hip Replacement procedure.
Aftercare appointments with Professor Kohan following your procedure include:
7 Days Post Surgery – This appointment is in order to check the skin cut & for Professor Kohan to asses your overall recovery.
14 Days Post Surgery – At this appointment the skin clips will be removed. An ultrasound will also be done by our radiographer in the rooms in order for Professor Kohan to check for blood clots.
6 Weeks Post Surgery – At this appointment Professor Kohan will asses the X-ray and monitor your overall recovery.
Consultations after this time attract a fee which is reimbursed in part from Medicare.
These fees should be discussed with the hospital directly. Please be sure to check with your health fund regarding a gap or out of pocket expenses.
If you are privately insured the prosthesis used in a Total Knee Replacement procedure is usually fully covered by your Health fund.
These fees are payable directly to the sonographer.
Phone
Locations
Bondi Junction
Suite 301C, 9 – 13 Bronte Road
Bondi Junction, NSW, 2022
