Anaesthesia and You
In the first place, we want to reassure you about the ability and qualifications of the anaesthetist who will manage you during surgery.
Anaesthetists in Australia are specialists – that is, they are among the world’s most highly trained doctors, having spent years undergoing specialist training in anaesthesia, pain control, resuscitation and managing medical emergencies.
The role of the Anaesthetist
People often think of anaesthesia as being put to sleep however, that’s not strictly true. Rather, the anaesthetist puts you in a state of carefully controlled unconsciousness. This is done so that surgery will be painless. No chance is taken during this period. All of your bodily functions are carefully and constantly monitored by your anaesthetist.
After your procedure we want you to experience as little pain and discomfort as possible and here again, the anaesthetist will help.
What should I tell the Anaesthetist?
The anaesthetist wants to have the best possible picture of you and your present conditions so that the most suitable anaesthetic can be planned.
This following information ensures all risks are kept to a minimum, safety and patient care is paramount.
- How healthy you are, if you have had any recent illnesses and also about any previous operations.
- Abnormal reactions to any drugs, or whether you have any allergies.
- Any history of asthma, bronchitis, heart problems or any other medical conditions.
- Whether you are taking any drugs at present- including cigarettes and alcohol- and, for women, whether they are on the pill.
- If you have dentures, caps or plates.
Is fasting really necessary?
We know the pangs of hunger can be severe but no food or drink 4hrs before the operation is a must. Not even water. If you don’t follow this rule, the operation may be postponed in the interests of your safety.
After the Operation
Your anaesthetist will continue to monitor your condition carefully well after surgery is finished to ensure your recovery is as smooth and trouble free as possible.
Once awake, you will feel drowsy. You may have a sore throat, feel sick or headache. These will soon pass.
To help the recovery process, you will be given oxygen to breathe, encouraged to take deep breaths and to cough. Only when you’re fully awake and comfortable will you be transferred either back to your room, or waiting area before returning home.
Do not worry if there is some dizziness, blurred vision or short term memory loss. It usually passes quite quickly.
Complications and risk factors
Some, infrequent complications include: bruising, pain or some injury at the site of injections, temporary breathing difficulties, temporary nerve damage, muscle pains, asthmatic reactions, headaches, the possibility of sensation, damage to teeth and dental prostheses, lip and tongue injury, temporary difficulty specking and epileptic seizure.
There can also be some very rare, serious complications including heart attack, stroke, severe allergic or sensitivity reactions, brain damage, kidney or liver failure, lung damage, paraplegia or quadriplegia, permanent nerve or blood vessel damage, eye injury, damage to the larynx (voice box) and vocal cords, pneumonia and infection of the blood transfusion.
Infections
Needles, syringes and intravenous lines are all used only once. They are new in the packet before your surgery commences and they are disposed of immediately afterwards. Cross infection from one patient to another is thus eliminated.
Blood Transfusion
A blood collection today from donors is carefully screened and tested but a very small risk remains. Hence, unless absolutely necessary, blood transfusions are not given.
Remember the possibility of serious complications including death is quite remote but does exist.
We urge you to ask questions. Your anaesthetist Dr Dennis Kerr will be happy to answer them and to discuss the best way to work with you for the best possible outcome.
Going Home
The best part is that most people now go home much sooner after surgery.
If you are having day surgery, make sure there is someone to accompany you home and for at least 24 hours don’t drive a car, make important decisions, use any dangerous equipment or tools, sign any legal documents or drink alcohol.
Your Role
There are some things you can do which make your anaesthetic safer:
- Get a little fitter- even a regular walk will work wonders.
- Don’t smoke- ideally, give it away six weeks before surgery.
- Drink less alcohol.
- Continue to take any medications which have been prescribed but remember to let your anaesthetist and surgeon know.
- If you are taking aspirin, consult your anaesthetist about whether you should stop taking it two weeks prior to surgery.
- If you are anxious and have questions make an appointment to see your anaesthetist before admission to hospital and get the answers you need.
- If you have any kind of health problem tell your anaesthetist and surgeon so they are fully informed.
What does it cost?
You should be aware that Medicare and Medical Fund rebates generally do not cover the entire costs of your anaesthesia. In other words, there will usually be a gap which you will be expected to pay. If you have any questions about costs please talk with your anaesthetist.
AMIS® FAQ
How long will my leg continue to swell and hurt?
The pain usually decreases rapidly during the first few weeks but the pain continues to improve for 12 months or even longer. The swelling is due to alterations in fluid return up the limb and will gradually diminish but may take 12 months or longer. Mobilisation helps. Exercise, stockings and elevation also help.
How much exercise should I do and how can I tell if I have done too much?
Mild and moderate exercise is beneficial but over-exercise is painful and possibly harmful. Generally the more active you are the better, but within limits.
When can I drive?
Driving is an individual matter. Some people regain their co-ordination and reflexes quickly and others take longer. Following hip surgery you should avoid driving for at least 2 to 3 weeks depending on your progress. Driving should not be considered if you are still taking pain medication.
When will I be able to go up and down stairs?
On the first day after surgery you should learn to walk up and down stairs with a physiotherapist at the hospital. The pace at which you regain agility on stairs depends on individual traits.
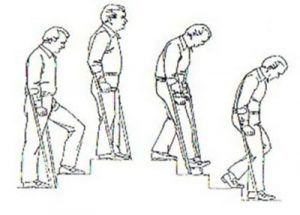
Up stairs: Take a step up with your good leg, then take the operated leg, followed by crutch or stick.
Down stairs: Place your crutch or stick first, then take a step down with the operated leg, followed by the good leg. Always go one step at a time.
What kind of shoes should I wear?
High heels should be avoided for the first 3 months otherwise there are no rules regarding shoes.
Should I use a heating pad or ice packs?
Both ice and heat can be used to help relieve pain but both can be harmful if left on too long. Never sleep with a heating pad on your hip as it can damage the skin and even cause a severe burn. Ice can be used several times a day. 20 minutes on and 20 minutes off is the usual regime.
How long should I continue taking my medications after surgery?
If iron is prescribed, it should be continued for 1 month after discharge from the hospital. Blood thinning medications (Aspirin) should be taken for 6 weeks. All pain medications may be taken as directed for pain. If you have any questions about your medications please ask.
Why do I have trouble sleeping at night?
Sleeping trouble is the most common question. You need patience. Surgical heeling takes approximately 6-8 weeks. Therefore you may be slightly uncomfortable for this time. Taking prescribed medication and applying ice can help. Also getting out of bed and moving the joint sometimes helps too.
Why don’t my legs feel equal in length?
This is a very commonly asked question. There are many reasons why you may feel a limb length discrepancy. During surgery, we used several methods to ensure limb length inequality, as best we can. Given current technology, probably, plus or -1 cm is about as accurate as we can get. Generally speaking, though, you need at least 1/2 cm or more before a permanent limp develops. This is because the spine of the pelvis can usually accommodate for the limb length inequality.
Another reason is that, before surgery, the hip is quite stiff. Over the years, you have gradually adapted to the stiff hip, by altering the angle of your pelvis and the spine. That is the new “” normal”” length with which you going to surgery. After the surgery, much of the stiffness is immediately resolved, and the limb can now extend fully giving you the feeling that it is longer. It feels longer, but in fact the length is the same as it was before surgery, it is just able to be extended fully.
We usually advise that you adopt a wait and see approach. Simply using the leg, walking, and gentle exercises as advised will allow the body skeletal system to adapt. This may take a year. However, if you use shoe raises, or insoles to make up for the perceived inequality, the body does not have a chance to adapt.
Phone
Locations
Bondi Junction
Suite 301C, 9 – 13 Bronte Road
Bondi Junction, NSW, 2022
